Russia’s mRNA Cancer Vaccine: A Revolutionary Leap in Cancer Treatment
Updated on : 09 January, 2025

Image Source: indiatoday.com
The announcement of a new cancer vaccine developed in Russia has generated significant excitement and hope within the medical community and among cancer patients worldwide. This innovative mRNA-based vaccine is set to be distributed free of charge starting in early 2025, marking a potential breakthrough in cancer treatment. This blog will explore the details surrounding the Russian cancer vaccine, including its development, mechanism of action, implications for patients, and its place within the global context of cancer research.
What Are Cancer Vaccines?

Image Source: cdn.cancercenter.com
Cancer vaccines are innovative immunotherapy treatments designed to stimulate the immune system to recognize and attack cancer cells. They fall into two main categories:
- Therapeutic Vaccines: These are intended for individuals already diagnosed with cancer. They work by exposing the immune system to specific antigens found on tumor cells, enhancing the body’s ability to identify and destroy these cancerous cells. Therapeutic vaccines can help stop tumor growth, eliminate residual cancer cells post-treatment, and potentially prevent recurrence.
- Preventive Vaccines: These vaccines aim to protect healthy individuals from developing cancer by targeting viruses known to cause certain cancers. A notable example is the human papillomavirus (HPV) vaccine, which helps prevent cervical cancer. By training the immune system to recognize viral antigens, preventive vaccines can significantly reduce cancer risk.
Overall, cancer vaccines represent a promising advancement in both treatment and prevention strategies in oncology.
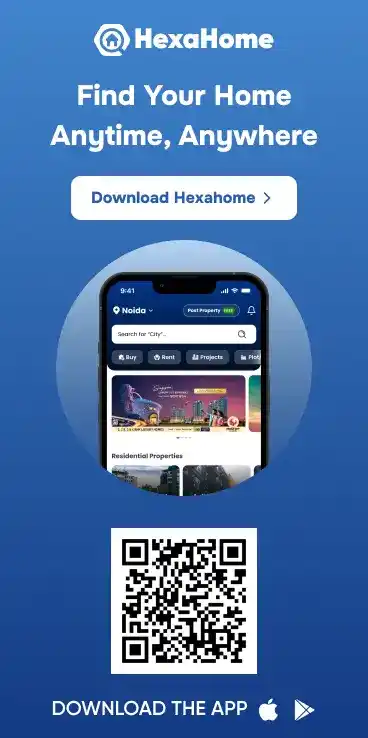
How Cancer Vaccines Work: Key Mechanisms of Action
Image Source: www.ucir.org
Cancer vaccines operate by enhancing the body's immune response to recognize and combat cancer cells, utilizing various mechanisms tailored to stimulate specific immune pathways.
Mechanisms of Action:
- Antigen Presentation: Cancer vaccines often include tumor-associated antigens (TAAs) or tumor-specific antigens (TSAs) that are presented to immune cells. Dendritic cells (DCs), as potent antigen-presenting cells (APCs), play a crucial role by processing these antigens and presenting them on their surface, activating T cells, particularly CD8+ cytotoxic T lymphocytes (CTLs) and CD4+ helper T cells.
- mRNA Vaccines: These vaccines introduce mRNA encoding TAAs into the body, leading to the production of antigens within host cells. The resultant antigens are presented on MHC molecules, stimulating a targeted immune response against tumor cells while minimizing damage to healthy tissues.
- In Situ Vaccination: This approach involves administering the vaccine directly into the tumor site, which activates local immune cells and induces an inflammatory response that recruits additional immune components to the tumor microenvironment, enhancing the overall anti-tumor effect.
- Viral-Based Vaccines: Modified viruses can be used to deliver TAAs directly into immune cells, triggering a robust immune response characterized by inflammation and cytokine release, further activating CTLs against cancer cells.
Through these mechanisms, cancer vaccines aim to slow tumor growth, prevent recurrence, and potentially eliminate early-stage cancers, representing a promising complement to traditional therapies like chemotherapy and radiation.
The Development of Russia's Cancer Vaccine

Image Source: jagran.com
Announcement and Expectations
On December 18, 2024, Russian officials announced the development of an mRNA-based cancer vaccine that is expected to be available for distribution free of charge by early 2025. Andrey Kaprin, General Director of the Radiology Medical Research Center of the Russian Ministry of Health, confirmed this news during a broadcast on Radio Rossiya. He emphasized that preclinical trials have shown promising results in suppressing tumor development and metastasis.
Collaboration Among Research Institutions
The vaccine's development is a collaborative effort involving several prominent institutions across Russia, including:
- Gamaleya National Research Center for Epidemiology and Microbiology
- Hertsen Moscow Oncology Research Institute
- Blokhin Cancer Research Center These institutions are working under state financing as part of a governmental initiative aimed at advancing domestic technologies in oncology.
Preclinical Trials and Future Prospects
- Current Status of Trials: As of late 2024, preclinical studies are ongoing, with initial results expected soon. The Russian Health Minister Mikhail Murashko indicated that clinical trials could begin shortly thereafter. These preclinical trials are crucial for assessing the vaccine's safety and efficacy before it can be administered to patients.
- Personalized mRNA Vaccines:
A significant aspect of Russia's approach is its focus on personalized mRNA vaccines tailored based on genetic analyses of each patient's tumor. This allows for a unique vaccine that teaches the immune system to target specific cancer cells effectively. Advanced computational methods utilizing artificial intelligence (AI) are facilitating this personalized approach, significantly reducing the time required to design these vaccines.
The integration of AI has reportedly enabled researchers to streamline the process of creating personalized vaccines, potentially reducing design time from several hours to less than an hour.
The Role of AI in Vaccine Development
Artificial intelligence (AI) plays a crucial role in the personalization of vaccines, particularly in the context of mRNA vaccines designed to target specific cancer cells or pathogens. This process involves tailoring vaccines to the unique genetic makeup of an individual's tumor or immune response profile, which enhances the efficacy of the treatment. AI contributes to personalization in several key ways:
- Identification of Epitopes: AI algorithms can analyze vast datasets to identify specific protein pieces (epitopes) that stimulate immune responses. By predicting which epitopes are most likely to elicit a robust immune reaction, researchers can design vaccines that are more effective for individual patients.
- Genomic Analysis: Through machine learning and computational models, AI can process genomic data from tumors to determine mutations that are present. This allows for the development of personalized mRNA vaccines that specifically target these mutations, thus improving the likelihood of a successful immune response.
- Dynamic Adaptation: AI systems can continuously learn from new data, allowing for real-time adjustments in vaccine design based on emerging research or patient responses. This adaptability is particularly important in rapidly evolving fields like oncology and infectious diseases.
Cancer Cases in India
Total Cancer Cases in India (2022)
| Category | Statistics |
|---|---|
| Estimated New Cancer Cases (2022) | Approximately 1,461,427 |
| Projected New Cancer Cases by 2025 | Estimated to rise to around 1,650,000 |
| Estimated Number of People Living with Cancer | Around 2.5 million |
| Estimated Annual Cancer-Related Deaths | Approximately 556,400 |
| Deaths in Age Group 30-69 Years | Total: 395,400 (71% of all cancer-related deaths) |
| Top Cancers in Men | Oral cavity and lung cancers |
| Top Cancers in Women | Cervical and breast cancers |
Leading Types of Cancer in India (2022)
| Type of Cancer | New Cases (2022) | Percentage of Total Cases |
|---|---|---|
| Breast Cancer | 192,020 | 13.6% |
| Oral Cavity Cancer | 143,759 | 10.2% |
| Cervical Cancer | 127,526 | 9.0% |
| Lung Cancer | 81,748 | 5.8% |
| Colorectal Cancer | 70,038 | 5.0% |
Cancer Cases Worldwide
Total Cancer Cases Worldwide
| Category | 2022 Statistics | 2050 Projections |
|---|---|---|
| Estimated New Cancer Cases | Approximately 20 million | Expected to rise to 35 million (a 75% increase) |
| Estimated Annual Cancer Deaths | Approximately 9.7 million | Expected to reach 18.5 million (an 89% increase) |
Leading Types of Cancer Worldwide in 2022
| Type of Cancer | New Cases (2022) | Percentage of Total Cases |
|---|---|---|
| Lung Cancer | 2.5 million | 12.4% |
| Breast Cancer | 2.3 million | 11.6% |
| Colorectal Cancer | 1.9 million | 9.6% |
| Prostate Cancer | 1.5 million | 7.3% |
| Stomach Cancer | 970,000 | 4.9% |
Trends in Cancer Vaccination

Image Source: gettyimages.com
Significant advancements and initiatives in cancer vaccination are underway globally, with particular emphasis on HPV vaccines and innovative cancer treatments. Here’s a summary of the current landscape:
HPV Vaccination Initiatives
-
Global Goals: The World Health Organization (WHO) aims for 90% of girls to be fully vaccinated with the HPV vaccine by the age of 15. This initiative is part of the broader goal to eliminate cervical cancer as a public health problem by 2100, which also includes screening and treatment targets.
-
Impact of Vaccination Programs: Current national HPV vaccination programs are projected to prevent approximately 818 cases of cervical cancer over the next 20 years. This highlights the effectiveness of vaccination in reducing cancer incidence.
-
Challenges in the Indo-Pacific Region: Despite the potential benefits, fewer than 10% of women in the Indo-Pacific have completed their HPV vaccination series. The Quad Cancer Moonshot Initiative aims to address these disparities by promoting vaccination and increasing access to screenings.
Innovative Cancer Vaccines
-
mRNA Cancer Vaccines: There is renewed hope for cancer vaccines, particularly those using mRNA technology. A notable example is the mRNA-4157 vaccine developed by Moderna and Merck, which is currently undergoing clinical trials for melanoma treatment. The FDA may grant approval for this vaccine by 2025.
-
Russia’s Personalized Cancer Vaccine: Russia has announced a groundbreaking mRNA-based cancer vaccine designed to treat existing tumors rather than prevent them. This vaccine will be distributed free of charge starting in early 2025, emphasizing personalized medicine approaches.
-
NHS Initiatives in the UK: The NHS has launched a Cancer Vaccine Launch Pad to expedite patient enrollment in trials for mRNA-based personalized vaccines targeting various cancers, including colorectal and pancreatic cancers.
Implications for Cancer Treatment
Potential Impact on Patients
The introduction of a free-to-access cancer vaccine in Russia has the potential to significantly transform patient care both domestically and globally. By eliminating the financial burden associated with cancer treatments, this innovative vaccine could enhance treatment adherence among patients who might otherwise avoid costly therapies. This accessibility is particularly crucial in a country where healthcare resources can be limited, allowing more individuals to receive cutting-edge cancer treatment without the stress of financial constraints.
The vaccine's anticipated launch in early 2025 is expected to improve outcomes for many patients, particularly those diagnosed with cancers that are currently difficult to treat. The focus on making this vaccine available free of charge aligns with broader public health goals of increasing access to essential medical innovations, potentially leading to earlier interventions and better overall survival rates.
Global Context
Russia's advancements in cancer vaccine development occur within a competitive global landscape where multiple countries and companies are racing to create effective cancer vaccines. Notable efforts include:
- United Kingdom: Collaborating with BioNTech, the UK is launching clinical trials for personalized cancer treatments that aim to tailor therapies based on individual patient profiles.
- United States: Companies like Moderna and Merck & Co. are developing experimental vaccines that have shown promising results against melanoma, one of the most aggressive forms of skin cancer. Recent mid-stage studies indicated that these vaccines could reduce the risk of recurrence or death from melanoma by half after three years of treatment.
This competitive environment underscores the urgency and importance of advancing cancer therapies globally. As countries strive to innovate and improve cancer treatment options, the introduction of Russia's mRNA-based cancer vaccine could serve as a catalyst for further research and development in this field. The collaborative efforts among various nations reflect a shared commitment to tackling one of the most pressing health challenges worldwide—cancer.
Challenges Ahead
Scientific Scrutiny and Validation
The development of mRNA cancer vaccines is subject to rigorous scientific scrutiny and validation as they progress from preclinical studies to clinical trials. Despite promising early results, several challenges must be addressed to ensure the vaccines are safe, effective, and applicable in real-world settings.
- Tumor Heterogeneity: One of the primary challenges is the inherent heterogeneity of tumors, which can vary significantly between patients and even within different regions of the same tumor. This diversity complicates the identification of universal antigens that can effectively stimulate an immune response across a wide patient population.
- Immunosuppressive Tumor Microenvironment: Many tumors create an immunosuppressive microenvironment that inhibits the activity of immune cells. This suppression can prevent the immune system from effectively targeting and destroying cancer cells, even if a vaccine successfully activates immune responses.
- Clinical Trial Outcomes: Current clinical studies have not consistently yielded remarkable outcomes, highlighting the need for ongoing research to refine vaccine formulations and improve patient selection criteria. The complexity of measuring immune responses and determining optimal dosing regimens further complicates the validation process.
- Regulatory Hurdles: As with any new therapeutic approach, mRNA cancer vaccines must undergo extensive regulatory review before they can be widely adopted. This process requires comprehensive data on safety, efficacy, and manufacturing consistency, which can be time-consuming.
Complexity of Cancer as a Disease
The complexity of cancer itself presents significant challenges to the development and implementation of effective vaccines:
- Cancer Cell Characteristics: Cancer cells often resemble normal cells, making it difficult for the immune system to distinguish between healthy and malignant cells. This similarity can lead to immune tolerance, where the body fails to mount an adequate response against cancerous cells.
- Finding Specific Antigens: Identifying cancer-specific antigens that do not also target normal tissues is a critical hurdle. If a vaccine targets antigens present on both cancerous and healthy cells, it can lead to adverse side effects by damaging normal tissues.
- Vaccine Delivery and Efficacy: Effective delivery of vaccines to the tumor site is another challenge. Factors such as poor vascularization in tumors and barriers posed by surrounding tissues can hinder vaccine efficacy. Additionally, determining the optimal timing for vaccine administration in conjunction with other treatments remains complex.
- Combination Therapies: The integration of cancer vaccines with other treatment modalities—such as chemotherapy or checkpoint inhibitors—requires careful planning and understanding of how these therapies interact. Identifying the best combinations and timing for administration is essential for maximizing therapeutic outcomes.
The Future Landscape of Cancer Vaccination
Increased Investment in Cancer Research
The cancer vaccine sector is experiencing a significant surge in investment, driven by the promising potential of innovative therapies and the urgent need for effective cancer treatments. As highlighted in recent analyses, the cancer vaccine landscape has seen a notable increase in funding, particularly for viral and nucleic acid-based vaccines, which have gained traction due to their rapid development capabilities and efficacy in eliciting immune responses.
- Funding Trends: Increased investment is not only coming from private companies but also from government initiatives aimed at advancing cancer research. This funding influx is expected to accelerate clinical trials and the development of new vaccine candidates.
- Emerging Technologies: Investment is increasingly directed towards cutting-edge technologies such as mRNA platforms, which have demonstrated success during the COVID-19 pandemic. This success has spurred interest in applying similar methodologies to cancer vaccines, potentially leading to breakthroughs in personalized medicine.
- Research Collaborations: The rise in funding has also facilitated collaborations between academic institutions, biotech companies, and pharmaceutical giants. These partnerships are crucial for sharing knowledge, resources, and expertise, ultimately enhancing the pace of innovation in cancer vaccine development.
Global Collaborations and Knowledge Sharing
The future of cancer vaccination is being shaped by global collaborations and knowledge sharing, which are essential for overcoming the challenges associated with cancer treatment. As countries and institutions work together, they can pool resources and expertise to expedite research and development efforts.
- International Partnerships: Collaborative efforts among countries are becoming increasingly common, with joint clinical trials and shared research initiatives aimed at developing effective cancer vaccines. For instance, partnerships between institutions in the United States, Europe, and Asia are focusing on harnessing diverse scientific perspectives to tackle complex challenges in cancer immunotherapy.
- Data Sharing Initiatives: Global data sharing initiatives are emerging as vital components of cancer research. By sharing clinical trial data, genomic information, and patient outcomes across borders, researchers can gain insights that lead to more effective vaccine designs and treatment strategies.
- Conferences and Workshops: International conferences dedicated to cancer research provide platforms for scientists to exchange ideas, present findings, and discuss advancements in vaccine technology. These gatherings foster collaboration and inspire new approaches to tackling cancer.
Regulatory and Policy Changes
As the landscape of cancer vaccination evolves, so too must the regulatory frameworks that govern vaccine development and approval.
- Streamlined Approval Processes: Regulatory agencies are increasingly recognizing the need for expedited pathways for promising cancer vaccines. Recent trends indicate a willingness to adopt more flexible regulatory frameworks that allow for faster evaluation of innovative therapies while ensuring patient safety.
- Policy Support for Research: Governments are implementing policies that encourage investment in cancer research and support the development of new treatments. This includes grants for research projects, tax incentives for biotech firms, and initiatives aimed at improving access to clinical trials for patients.
- Ethical Considerations: As personalized medicine becomes more prevalent, ethical considerations surrounding patient consent, data privacy, and equitable access to therapies will need to be addressed. Establishing clear guidelines will be essential to ensure that advancements in cancer vaccination benefit all patients fairly.
Conclusion
The journey toward effective cancer vaccination is fraught with challenges but also filled with promise. As Russia prepares to launch its mRNA cancer vaccine in early 2025, it stands at the forefront of a potential revolution in oncology that could reshape how we treat this pervasive disease.
With ongoing research and collaboration across borders, there is hope that advancements like these will not only improve survival rates but also enhance quality of life for millions affected by cancer worldwide. As we anticipate further developments in this field, it remains crucial for stakeholders—scientists, healthcare providers, policymakers, and patients—to work together towards achieving comprehensive solutions in combating cancer through innovative technologies like mRNA vaccines.